Table of Contents
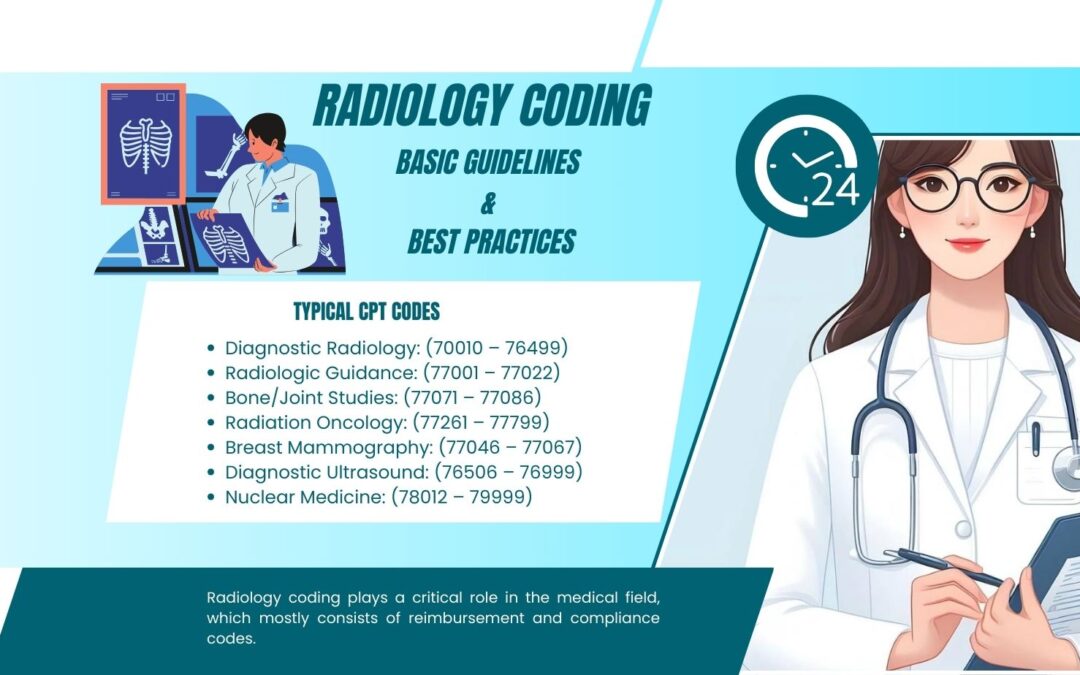
Radiology coding plays a critical role in the medical field, which mostly consists of reimbursement and compliance codes. The medical imaging services are subtle; it is critical to follow the current coding requirement and other best practices to avoid claims processing failure. Medical coding services offer healthcare providers a realistic means of assuring accurate utilization of radiology procedure codes, given the diverse range of imaging techniques. For appropriate radiology coding, one must have a thorough awareness of the CPT and ICD codes for various imaging modalities and unique diagnostic requirements.
Here we will explain the essential thoughts and regulations of radiology coding, discuss the major challenges, and provide helpful tips on billing standards, best practices, and how to avoid traps that may impede the operation of radiology departments’ revenue cycles.
What is Radiology?
Radiology is a medical specialty that conducts and interprets imaging techniques such as
- X-rays
- Computed Tomography (CT)
- CT Angiography (CTA)
- Magnetic Resonance Imaging (MRI)
- MR Angiography (MRA)
- Ultrasound, (generates images of interior organs using sound waves)
- Fluoroscopy
- Nuclear Medicine, (concentrates on radioactive material imaging)
- Positron Emission Tomography (PET) scans
Radiologists utilize these procedures to help diagnose and treat patients with diseases or health issues. Individual payers may have their own set of restrictions, which complicates and slows down the billing process. The proper medical necessity method ensures that the secretary/green MHS collects all relevant clinical data before providing a service. It also validates conformity with coding practices when an examination and certain paperwork are completed. Radiology codes are frequently changed. Therefore, you have to be updated with new codes to prevent billing problems. Resources like the CPT® code book and regular training can be beneficial. Precise coding accurately records the services rendered, assuring reimbursement.
Typical CPT codes
Diagnostic Radiology: (70010 – 76499)
Radiologic Guidance: (77001 – 77022)
Bone/Joint Studies: (77071 – 77086)
Radiation Oncology: (77261 – 77799)
Breast Mammography: (77046 – 77067)
Diagnostic Ultrasound: (76506 – 76999)
Nuclear Medicine: (78012 – 79999)
Document Review to Determine Diagnosis Code
To determine the diagnosis code, it is necessary to review two essential documents. Each is a potentially useful source material for selecting a diagnosis code for the meeting. One can:
- Test order and associated signs/symptoms
- Radiology report with the final written interpretation.
Although diagnosis coding for diagnostic radiological exams appears to be a simple procedure, it is not always so. Often, documentation that must be reviewed before issuing a diagnosis code is unavailable or imprecise, resulting in confusion and contradiction. Furthermore, problems pertaining to under- and up-coding must be addressed. These problems may lead to incorrect invoicing and noncompliance with regulatory requirements.
Diagnostic Test Order
The radiology coding process starts with a test order from the concerning physician, which is delivered to an imaging center, hospital, or other diagnostic imaging service provider. Medicare only pays for services that are reasonable and necessary, thus, having a thorough and precise test order is essential to coding compliance.
The CPT code is an acronym for Current Procedural Terminology, which is maintained by the American Medical Association. This standard facilitates the accurate identification and documentation of medical treatments or services. A proper medical necessity screening procedure ensures that all relevant clinical data is obtained before providing a treatment.
If this information is missing, the person who ordered the exam should be questioned about it before proceeding. Even if a radiological report identifies and explains an aberrant finding or disease, the symptoms are critical in determining if it is incidental (discovered but unrelated) or related to the original investigation. Furthermore, a test requested to “rule out” a particular disease is treated as a screening exam by Medicare. If there are no documented signs or symptoms, it will be coded and billed as follows:
The first diagnostic is assigned a screening code (such as V72.31), and subsequent diagnoses contain any discoveries discovered during the process, such as abnormal test results. If the referring physician uses words that indicate uncertainty (e.g., probable, suspected, questionable, rule out, or working), the diagnosis should not be classified.
The report on radiology
Determining if particular conditions listed in the results section or impressions are clinically imperative or just coincidental findings will be made easier with a thorough analysis of the clinical indications. Radiology reports have four primary sections:
- Clinical indications
- Technique
- Summary of findings
- Impression and final interpretation
The radiologist’s final interpretation, the impression, may identify many disorders and is the final piece of the puzzle in determining a primary diagnosis code.
Radiology Coding’s Major Obstacles
Radiology coding depends heavily on accurate documentation. The complexity of codes makes it challenging to effectively write particular operations since they include several components. Make sure all reports are comprehensive and include pertinent information. Some procedures should be bundled under a single code. Always check the National Correct Coding Initiative (NCCI) edits to avoid unbundling errors. Appropriate documentation bolsters the selected codes, reducing differences with insurers. There are discrepancies in the guidelines amongst insurers, which results in inconsistent claims. Erroneous coding may set off audits, which may lead to monetary losses and harm to one’s reputation.
In today’s environment, technology is an unbeatable strength. It is decisive to the transformation of many industries, including healthcare. The incidence of discrepancies in codes is decreased, and coding policies are adhered to when technology is implemented properly and carefully used in conjunction with coding software solutions equipped with coding prompts, integrated systems for validation checks for enhanced coding, and electronic code lookup.
Solutions for Radiology Billing and Coding
Radiology coding is a difficult procedure that needs accuracy. It has authority to decide how effective your claims are. It is not a task for the inexperienced or untrained to code. Claims that are successfully coded can increase in number and decrease in denials. Accurate coding denotes accurate billing for every patient’s care, consultation, and prescription.
On the other hand, errors or delayed coding could result in denials, which would cause a revenue bottleneck. If one is aware of all the code updates and challenges that their practice or hospital faces, they can prevent these expensive mistakes. A comprehensive radiological report guarantees that the codes you and your business select are appropriate. Precise coding allows the healthcare facility to receive maximum income. The signs and/or symptoms that prompted the test may be recorded as extra diagnoses if they are not fully explained or related to the confirmed diagnosis.
Wrap Up
It is critical to handle radiology coding carefully, as it translates medical imaging services into standardized codes. Healthcare providers can decrease denials and increase compliance by closely monitoring test orders, radiology repositories, and accurate invoicing and reimbursements. They should also stay informed about any changes to codes. Revenue can be increased by using these coding and billing techniques. Additionally, they improve radiology techniques in general.
Read More: Telehealth Urgent Care: Your Digital Gateway to Speedy Medical Attention