Table of Contents
Modifier 74 Description
In the intricate world of medical billing, modifier 74 plays an integral role, particularly in cases involving surgical or diagnostic processes. Knowing when to use this modifier 74 is crucial to ensuring correct payment and adherence to insurance regulations. In the particular situations, the use of Modifier 74 is critical to making effects on the medical billing claims procedure.
What is Modifier 74?
Modifier 74, also known as Discontinued outpatient Hospital/Ambulatory Surgery Center (ASC) surgery After Anesthesia Administration is used when a surgery is terminated after the patient has received anesthesia. The essential issue here is that the anesthesia had to be fully induced before the procedure was terminated. This modifier informs the payer that the procedure was ended for reasons beyond the healthcare provider’s control, yet considerable resources were consumed up to the point of termination.
When to Apply Modifier 74 in Medical Billing?
Understand certain situations when Modifier 74 should be applied. This modifier is appropriate in the following circumstances:
- Modifier 74 is most commonly used when a surgical or diagnostic procedure is reduced or discontinued owing to unexpected difficulties. These complications could be connected to the patient’s health, like a rapid drop in blood pressure, heart problems, or unusual reactions to anesthetic. In such cases, the medical team decides to halt the diagnostic procedure in the interest of the patient’s safety.
- Another situation is that continuing the diagnostic procedure may endanger the patient’s health. If the surgeon or physician determines that the patient’s condition is deteriorating or that the procedure would cause irreversible injury, the procedure may be stopped. Even though the treatment is not yet complete, tremendous effort and medical resources have been expended up to this point.
- Unexpected findings during a diagnostic procedure may cause the surgeon to stop the process. For example, if a diagnostic operation discovers a disease that necessitates a different strategy, the current procedure may be stopped and postponed for a more suitable intrusion. In such circumstances, Modifier 74 can be used to indicate that the surgery was interrupted but the anesthetic and surgical preparation were finished.
Modifier 74 Reimbursement?
When Modifier 74 is applied correctly, healthcare practitioners can earn partial compensation for an operation that was halted and not completed. It acknowledges the utilization of resources such as anesthetic, operating room time, surgical preparation, and staff contribution. However, the reimbursement rate may be changed based on the payer’s policy for partially completed treatments.
Modifier 74 is subject to specific guidelines from the majority of insurance payers, including Medicare and Medicaid. It is critical to adhere to their policies meticulously, as misuse or inappropriate implementation of this modification might result in claim denials or delayed payments. Billing personnel should verify that the relevant paperwork is included with the claim to support the rationale for terminating the operation.
Documentation necessities for Modifier 74
When using Modifier 74, it is imperative to provide accurate and complete documentation. The clinical justification for stopping the surgery, the steps performed before anesthesia was administered, and the reasons why the procedure was stopped should all be included in the modifier 74. Document the following critical points:
- Patient condition before, during, and after anesthetic induction.
- Reason for discontinuation, such as problems or unexpected findings.
- Clinical decision-making process that resulted in the procedure’s halt.
- Confirmation that anesthesia was delivered before the surgery was terminated.
Providing this degree of detail ensures that the claim is processed efficiently, lowering the likelihood of a denial or request for additional information.
Most Common Mistakes to Keep Away of When Using Modifier 74
When utilized properly, Modifier 74 can be very helpful, but billing teams and healthcare practitioners should stay away from these common blunders:
Anesthesia must have been given, one of the most important requirements for applying Modifier 74. In the operation process that was stopped before anesthesia was administered, Modifier 73 (Discontinued Outpatient Operation Prior to Anesthesia Administration) ought to be applied. Claims may be rejected or reimbursement may be erroneous if the improper modifier is applied.
Modifier 74 is attached with detailed and explicit documentation for insurance payers. The claim could be rejected in the absence of adequate paperwork outlining the reasons why the procedure was stopped. It includes any pertinent clinical notes from the surgeon or anesthesiologist in the medical records, along with a clear explanation of the reason for cessation.
Different payers may have different rules regarding the use of Modifier 74. It’s important for billing teams to be familiar with the specific policies of each payer to avoid errors. Some insurance companies may have stricter requirements for documentation or may reimburse at different rates for discontinued procedures. Always verify the payer’s guidelines before submitting a claim with Modifier 74.
It is possible that various payers have different guidelines for using Modifier 74. To prevent common mistakes, billing teams should be familiar with each payer’s unique policies. Certain insurance companies might have more stringent paperwork requirements or offer varying reimbursement rates for discontinued procedures. Always check the payer’s instructions before using Modifier 74 to submit a claim.
Key Differences Between Modifier 73 and Modifier 74
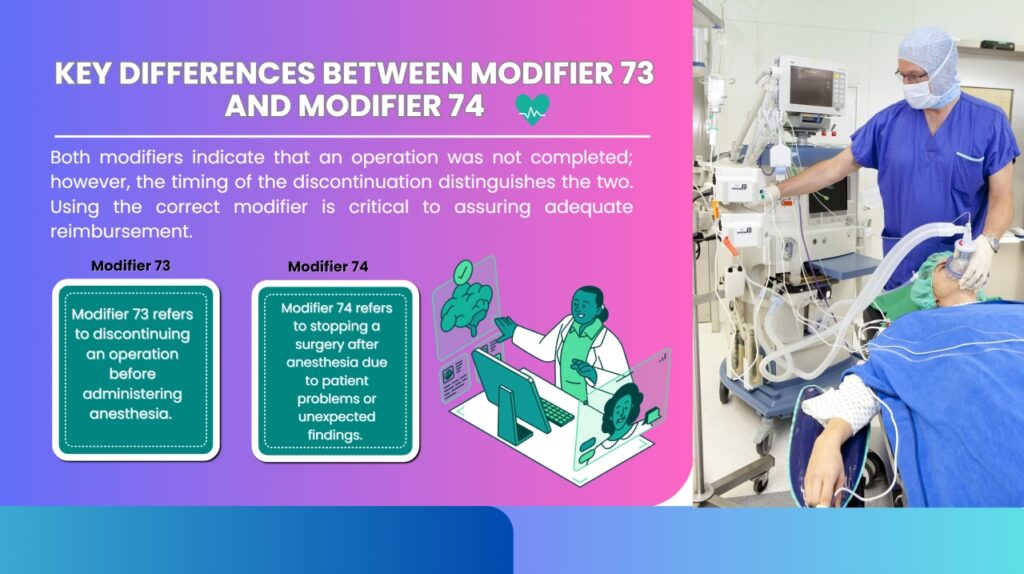
It’s crucial to differentiate between Modifier 73 and Modifier 74 to ensure accurate billing practices. Here are the main differences:
- Modifier 73 refers to discontinuing an operation before administering anesthesia. This modification is often utilized when the patient’s health changes before the anesthetic process begins or when the operation cannot be completed owing to other extenuating circumstances. For example, an inguinal hernia is present in a patient who is 56 years of age. It opens the hernia. Prior to surgery, the patient is brought to the operating room, and before general anesthesia is given, the patient’s blood pressure is elevated. The supplier decides to halt the process as a result of this investigation. In this instance, apply modifier 73 to the right CPT® code.
- Modifier 74 refers to stopping a surgery after anesthesia due to patient problems or unexpected findings. For example, the lithotripsy, stent, and cystourethroscopy equipment are displayed to a patient who has the necessary calculator. A general anesthetic is administered, and the patient is prepared. included; however, the severity is constant, and the provider ends the operation after a few tries by deleting the instance. In this instance, apply modifier 74 to the right CPT® code.
Therefore, both modifiers indicate that an operation was not completed; however, the timing of the discontinuation distinguishes the two. Using the correct modifier is critical to assuring adequate reimbursement.
Multiple Processes
If many procedures are planned but not carried out, just the major surgery with an appropriate replacement (73 or 74) is recorded. If one process is complete and another has begun but not yet completed, report the second process using modifier 74 and code the first process without modifier. There is no reporting of other scheduled procedures that have not yet begun.
Substitution 73 is applicable to a maximum of one procedure code that the patient has encountered. Thus, switch 73 can only report the one-way process (first page) when planning and terminating a two-way process. It is not possible to report the second page. Binary changes 50 and 73 should not be reported in the same procedure code.
Wrap Up:
Modifier 74 is a crucial component in medical billing that compensates healthcare professionals for partially finished treatments once anesthetic is delivered. Correct use of modifier necessitates a thorough grasp of the precise conditions in which it applies, as well as extensive documentation to back up the assertion. Healthcare providers can ensure that their claims are processed quickly and correctly by following payer guidelines and avoiding common errors.
Read More: Best Strategies to Boost Patient Satisfaction in Healthcare
Reference 1,